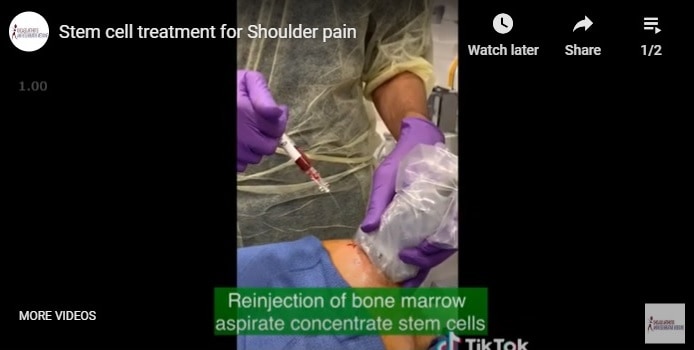
May 31, 2020 | Blog, regenerative medicine, Regenexx, Rotator Cuff, Rotator Cuff Tendinitis, Shoulder, Stem Cells, Tendinitis, tendonitis
Shoulder stem cell treatment. Stem cell treatment for Shoulder pain. Bone marrow aspirate concentrate stem cell treatment for shoulder labral tear and rotator cuff tear. #shoulder #shoulderpain #labraltear #rotatorcufftear #prp #stemcell #regenerativemedicine ***For...
May 25, 2020 | Blog, Rotator Cuff, Rotator Cuff Tendinitis, Shoulder
We have quite a few non surgical treatment options for shoulder pain, including for shoulder arthritis, rotator cuff tendinitis, shoulder tendon tear, and shoulder injuries. In this case a suprascapular nerve block gave this patient pain relief and allowed her...
Apr 26, 2020 | Ankle, Arthritis, Blog, Hip, Knee, lower back pain, Osteoarthritis, Regenerative, regenerative medicine, Shoulder, Tendinitis, tendonitis, Wrist
Inflammation, Pain, and Musculoskeletal Health Inflammation is complicated. But it definitely has a role in musculoskeletal health, pathology, and pain. Hello, this is Siddharth Tambar from Chicago arthritis and regenerative medicine. On this video today I am talking...
Apr 18, 2020 | Arthritis, Blog, Knee, Ligament, lower back pain, Osteoarthritis, Prolotherapy, PRP, Regenerative, regenerative medicine, Regenexx, Shoulder, Stem Cells, Tendinitis, tendonitis
Joint Stability- Your Musculoskeletal Health. Stability, Tensegrity, and Biotensegrity are key aspects of musculoskeletal health that you must understand. The opposite, instability, leads to progressive stress and damage in your joints and tendons. Hello, this is...
Mar 4, 2020 | Blog, PRP, regenerative medicine, Rotator Cuff, Rotator Cuff Tendinitis, Shoulder, Stem Cells
If you have shoulder pain, this video discusses regenerative medicine treatment options including stem cell and prp treatments....

Feb 15, 2020 | Blog, Regenexx, Rotator Cuff, Rotator Cuff Tendinitis, Shoulder, Stem Cells
Treating a shoulder rotator cuff tear with your own bone marrow stem cells is a novel and exciting idea. A recent study showed the effectiveness of this for partial thickness rotator cuff tears. —————————————————— Article: A Randomized Controlled Trial of the...